Last Friday, I participated in a roundtable discussion in Washington, D.C. conducted by the Aspen Institute's Sports & Society program called "Playing Safety: The Future of Youth Football?" It was moderated by ESPN's Tom Farrey and, in the phrase made famous by the movie Casablanca, rounded up all the usual suspects on concussion safety and football, including MomsTEAM concussion expert emeritus Dr. Bob Cantu, USA Football Executive Director Scott Hallenbeck, and NFL Player Association President DeMaurice Smith, among other luminaries from the world of football and journalism. I was indeed honored to be asked to join those debating the future of the sport.

Although the participants admittedly came to the table viewing football and concussion safety through the prism of their own experience and advancing the narrow interests of the organizations they represented, the roundtable was a valuable exercise, even though I'm pretty sure almost everyone left the meeting still hewing to the same views they had coming in. But the goal wasn't to change minds (if it was, it didn't meet that almost impossible challenge.) Instead, as the saying goes in diplomatic circles when a consensus can't be reached, what took place was, at its best, a "full and frank discussion" of the issues.
As I knew would be the case going in, a number of the participants came out strongly against the playing of tackle football before the age of 14, or said they would personally never let their child play football, period. As was also to be expected, the no-football-before-14 group, led by Bob Cantu, encountered push-back from USA Football's Hallenbeck, Pop Warner's Jon Butler, NFLPA President Smith, and NFL Senior Vice President Jeff Miller, among others.
When I finally had a chance to speak, we were already running over the 2 1/2 hours allotted for the roundtable, so I was only able to briefly touch on two of my many message points: one, that the game can be and is being made safer, and two, that, based on my experience following a high school football team in Oklahoma this past season - which will be the subject of a MomsTEAM documentary to be released in early 2013 called The Smartest Team - I saw the use of hit sensors in football helmets as offering an exciting technological "end around" the problem of chronic under-reporting of concussions that continues to plague the sport and remains a major impediment, in my view, to keeping kids safe (the reasons: if an athlete is allowed to keep playing with a concussion, studies show that their
recovery is likely to take longer, and they are at increased risk of
long-term problems (e.g. early dementia, depression, more rapid aging of the brain, and in rare cases, chronic traumatic encephalopathy, and in extremely rare instances, catastrophic injury or death. )
Some expressed the view that a decline in participation in youth, junior high and high school football is inevitable. I am not one of those who is in that camp, either.
Some also said it was inevitable that research would eventually lead us to one ineluctable conclusion: that football poses an unacceptable level of risk of long-term injury. Again, while I am not a scientist or medical doctor, I don't necessarily agree, especially if the amount of what Bob Cantu calls "total brain trauma" can be significantly reduced through a combination of limits on full-contact practices and/or hit counts, rule changes, and if we do a better job of identifying concussive injury to get concussed players off the field (or ice, or field, or court, or pitch), and and hold kids out longer before they are allowed to return to play so the risk of reinjury is reduced as much as reasonably possible.
Instead, I predict that we will ultimately learn that football and other contact and collision sports with high concussion rates do not pose an unreasonable risk of harm to the vast majority of athletes (especially those whose football careers end after high school), and that, while it may take a while, we will eventually learn to identify those athletes who, because of genetic predisposition or environmental factors, are at greatest risk, so that they and their parents can intelligently assess the level of risk and decide whether football is right for their family.
No need to panic
What continues to be lost, in my view, in much of what the media has reported over the last six years about the results of autopsies conducted by researchers at the Sports Legacy Institute in Boston on the brains of athletes - autopsies which show the presence of the dark splotches of tau protein which are the tell-tale sign of CTE - which is that they provide, at most, anecdotal evidence suggesting a possible connection. There are no studies that show a statistically significant increase in the likelihood of CTE simply from playing football or other contact or collision sport, and none, as far as I know, are even in the research pipeline, but those who say it is too early to connect the dots, well, their voices are being drowned out by those who suggest exactly that.
Could it be that the athletes found by SLI to have CTE were genetically predisposed to developing Alzheimer's and aren't representative in any way shape or form of the general population but, instead, of the small percentage of vulnerable ones? In other words, that not everyone who plays sports is destined to develop CTE. How many millions of men in their twenties, thirties, forties, and beyond, have played football without enduring cognitive damage?
While a 2012 study by researchers at the University of Michigan suggests that concussions may speed up the brain natural aging process, the long-term effect of a concussion, even two or three, remains unclear.
"The last thing we want is for people to panic. Just because you've had a concussion does not mean your brain will age more quickly or you'll get Alzheimer's," said lead author of the study, Steven Broglio, Assistant Professor of Kinesiology and Director of the Neurotrauma Research Laboratory at Michigan. "The influence of various lifestyle and environmental factors, such as smoking, alcohol consumption, physical exercise, family history (genetics), whether or not a concussed athlete 'exercises' their brain, and even how dense the gray matter in a person's brain is, which gives them greater 'cognitive reserve' to draw upon may also impact the brain's aging process," he said, such that "concussion may only be one small factor."
In addition, Broglio said, this line of research is still in its infancy. "'It's not entirely clear," he recently told the Kalamazoo News, "if and how the brains of young athletes are affected by the sports they play. 'We are realizing it's probably not how many concussions you have that makes a difference, but the total exposure' to concussive and sub-concussive blows."
So does Broglio think that if an athlete sustains a single concussion in high school, it means they will get dementia at age 50? "Clinically, we don't see that. What we think is it will be a dose response," Broglio said.
"So, if you played soccer and sustained some head impacts and maybe one concussion, then you may have a little risk. If you went on and played in college and took more head balls and sustained two more concussions, you're probably at a little bigger risk. Then if you play professionally for a few years, and take more hits to the head, you increase the risk even more. We believe it's a cumulative effect."
So what's Broglio's answer to my earlier question: Does the average high school athlete face risks similar to those of former professional football players - such as those whose brains, upon examination after death, show signs of chronic traumatic encepholapathy (CTE), or who, even if still alive, exhibit signs of serious depression or early-onset dementia, which researchers have linked to their years on the playing field?
Broglio says that there is little to no evidence that they do. "We're not seeing an epidemic of men in their early 50s with early Alzheimer's because they played high school football,"
Play smart, not scared
When all is said and done, I continue to believe that, instead of sensationalizing and scaring parents, the media, not to mention the scientific and football communities, should take a much more balanced approach, one which recognizes that (a) the research is a long way from establishing that football or any contact or collision sport leads to a statistically greater risk of chronic traumatic encephalopathy, early dementia or Alzheimer's; (b) helmet-to-helmet contact can be dramatically reduced through the teaching of proper tackling and rules against such contact; and (c) long-term adverse health effects can be limited through better identification of concussive injury, immediate removal from play of those with suspected concussion, cognitive rest after injury, and more conservative return-to-play guidelines.
Specifically, I believe the following five steps, among others, can help make the game safer:
1. Make safety training and the teaching of proper tackling mandatory for coaches: In order to coach youth or high school football a coach should be required to be certified in concussion safety and safe tackling training. The reasons are clear:
- 76% of coaches in a 2012 Safe Kids Worldwide survey said they wanted more concussion training, but fully 40% admitted that they have no safety training at all;
- An alarming half (52%) of all coaches mistakenly believe that there is an acceptable amount of head contact (ie. getting their "bell rung", seeing stars) young athletes can sustain without potentially causing a serious brain injury, with the percentages of those who felt this way highest among coaches under age 35, male coaches, and paid coaches; and
- Nearly half (47%) agreed with the statement that they had so many other responsibilities as coaches and so little time that they could not focus on injury prevention.
2. Make sure helmets fit. Making sure that football helmets fit properly, and that those with air bladder linings are properly inflated, may be two of the simplest but most effective ways to minimize the risk of concussion and catastrophic brain injury. A recent study shows that, while properly fitting helmets don't necessarily reduce the risk of concussion, the risk goes way up if the helmet doesn't fit properly. This is the reason behind the new NFHS rule this fall requiring a player whose helmet comes off to sit out a play. Kids need to wear lighter helmets specifically designed for their smaller heads and weaker necks. There are new youth-specific helmets coming on the market, and more are sure to follow. Also, football programs should not put all their helmets eggs in one basket: because one size does not fit all, they should offer at least two different types of helmets to ensure proper fit.
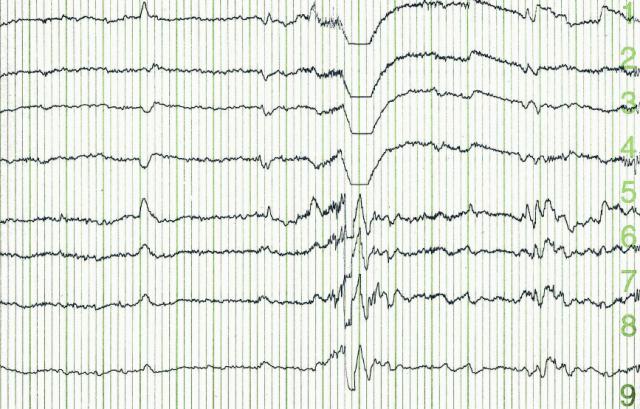
3. Use "hit sensors." Widespread use of accelerometers - whether they be inside the helmet, in a sweatband, or in the chinstrap, and transmitting data wirelessly to the football sideline on hits that might result in concussion, will help combat the chronic under-reporting of concussions resulting from the reluctance of players to self-report symptoms and the inability of sideline personnel and game officials to spot a concussed player. Hit sensors are needed at every level (including the NFL, where I know the players' union is currently against them), but especially at youth and high school level. There are lots of companies which have already brought or will be bringing hit sensors to the market, and I am excited about their potential in revolutionizing the identification of concussive injury, which could go a long way to making the sport safer, in my view. The athletic trainer of the Oklahoma high school team we are featuring in The Smartest

Team documentary told us he was glad sensors were in the helmets to alert him to a hit of sufficient g force that it that might cause concussion. Likewise, the players said the presence of a hit sensor relieved them of the responsibility to report concussion symptoms themselves, something that they, like most players, candidly admit they are reluctant to do. Widespread use on the sports sideline of the King-Devick test, which studies are showing can quickly identify on the sports sideline those athletes who should not be allowed to return to play and instead referred for further evaluation, and which can be administered in about two minutes by just about anyone, whether they be parent, coach, or athletic trainer), could also go a long way in solving the concussion identification riddle.
4. Reduce the number of full-contact practices at the high school level. The NFL only allows one contact practice a week; the Ivy League, two. Steps have been taken by Pop Warner and USA Football to limit contact practice time at the youth level. Yet there is no limit on the number of full-contact practices at the high school level. Mandating such a limit would dramatically reduce total head trauma, including the accumulation of sub-concussive hits that researchers at Purdue in a 2010 study found can lead to subtle cognitive deficits that evade detection via the usual signs or symptoms method.
5. Better strength and conditioning, particularly of neck muscles. Younger players, as Bob Cantu points out, have weaker neck muscles. MomsTEAM's concussion expert, Dr. Bill Meehan, Director of the Sports Concussion Clinic at Children's Hospital Boston, and author of Kids, Sports, and Concussion, thinks one way that may reduce the risk of head injury is to strengthen the neck muscles so they better cushion against impact.
At a tipping point?
The differences of opinion at the Aspen conference were stark and sharply drawn. There were many in the room, of course, who don't share my views in the slightest. But "sooner or later," predicted Bill Mayer, owner of the UFL's Virginia Destroyers, we will reach what Malcom Gladwell calls the tipping point. "Tipping points," said Mayer, "are usually reached because there is some person that has an abnormal amount of influence in the opinion of others. Who it is, that person is probably in this room."
Who will it turn out to be?
Stay tuned.
Note: For the video of the roundtable which appeared on C-SPAN2, click here.
Brooke de Lench is the Founder and Publisher of MomsTEAM.com, author of
Home Team Advantage: The Critical Role of Mothers in Youth Sports, and Executive Producer of the forthcoming football documentary,
The Smartest Team, slated for release in early 2013.